Bacterial Vaginosis - The Era of Treating Male Partners Has Arrived
A look at recurrent BV and a fantastic new study
Bacterial vaginosis or BV is the most common cause of abnormal vaginal discharge, and over their lifetime, up to one-third of women will have this infection at least once.1-3 The most common symptoms are discharge, odor, and irritation. Awareness of BV is essential not only because the symptoms are bothersome, but it is associated with a variety of health consequences, such as an increased risk of preterm labor and increased acquisition of HIV and other sexually transmitted infections (STIs) if exposed.1
Adding another layer of complexity to bacterial vaginosis is its propensity for recurrence. While some women may only have it once or twice, many suffer from multiple recurrences, and the exact reasons are unknown. The risk of recurrence within a year is high–66% will have a recurrence within the first year after treatment.1-3
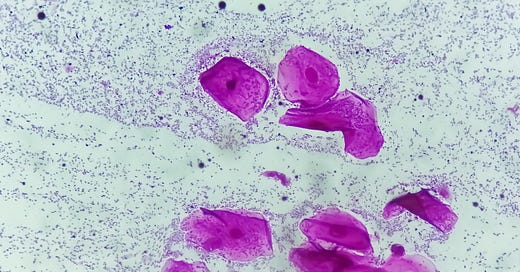
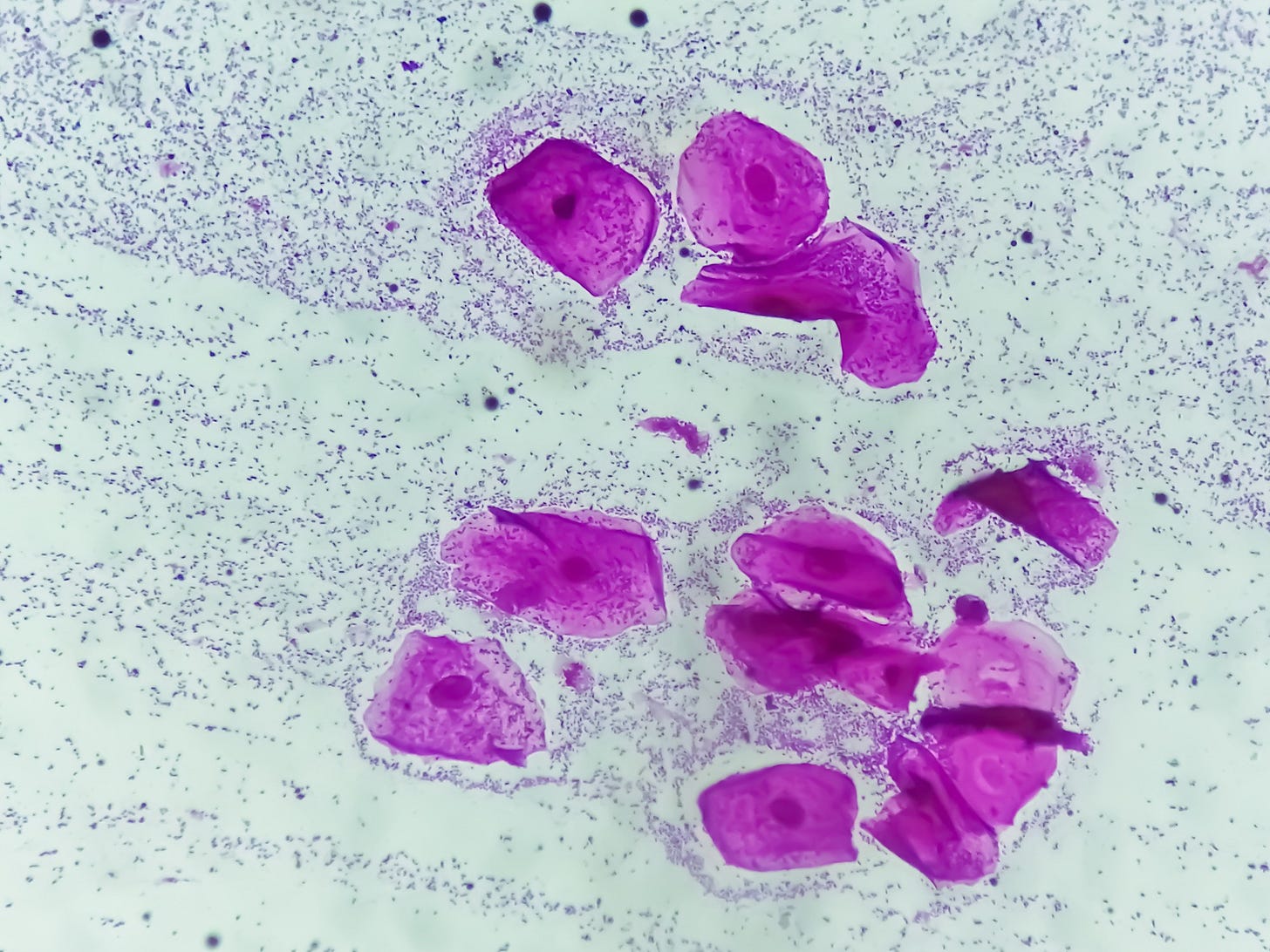
Bacterial vaginosis is dysbiosis, which is a shift or change in the composition of the microbiome. With BV the bacterial ecosystem in the vagina shifts from a platform dominated by lactic acid producing lactobacilli, to one dominated by anaerobic bacteria; in essence, it is a shift from a healthy microbiome to one dominated by bacteria that can cause problems.
The specific cause or causes of BV aren’t known. For example, with chlamydia, we know that exposure to the bacteria chlamydia trachomatis is required to cause an infection, but it’s not that simple with BV. There are bacterial vaginosis associated bacteria (BVAB), such as Gardeneralla vaginalis and Atopobium vaginae, but it requires more than just the bacteria to develop BV.1,2 One thing that has emerged as an essential step is the presence of a biofilm, a community of microorganisms that adheres to surfaces and is encased in material that protects them from the immune system and antibiotics.1,2 Biofilms help perpetuate the infection by optimizing growth conditions for the bacterial vaginosis associated bacteria (BVAB), but also, they shield the bacteria from the immune system or antibiotics.
There has actually been a fair bit of research into bacterial vaginosis, but despite this, progress has been slow, almost certainly in part due to the complexity of the condition. Although, if COVID-19 taught us anything, it’s that if you throw a shit ton of money at a problem, results are more likely. For example, a lot of money was spent on COVID-19, and we went from sequencing the virus at the beginning of 2020 to having vaccines (plural) by the end of the year.
Bacterial vaginosis is believed to be sexually transmitted, for women who have sex with men as well as women who have sex with women, but this isn’t understood in the way that we understand transmission of chlamydia or HIV. We know that condoms reduce the risk of BV for women who have sex with men, and the penis of a male partner of a women with BV is more likely to have bacterial vaginosis associated bacteria (BVAB), studies looking at treating male partners with oral antibiotics have been disappointing.4,5 However, a new study looking at treating male partners with an oral AND a topical antibiotic for the penis has yielded some impressive results.
The study, “Male-Partner Treatment to Prevent Recurrence of Bacterial Vaginosis,” by Vodstrcil et. al, was published this week in the New England Journal of Medicine.6 In the study, women with bacterial vaginosis who were in a monogamous heterosexual relationship for at least 8 weeks were treated with the appropriate antibiotic therapy for bacterial vaginosis (oral metronidazole, vaginal clindamycin, or vaginal metronidazole gel). Their male partners were then enrolled, and randomized to either no treatment or metronidazole 400 mg twice a day for 7 days and 2 cm of 2% clindamycin cream applied to the glans penis and the upper shaft (and under the foreskin if not circumcised) twice a day for 7 days. Couples were advised to abstain from sex for the 7 days of penile treatment. The men in the control group were not given a placebo gel as there was a concern that could theoretically impact the penile microbiome.
The investigators set out to enroll 290 couples. However, an interim safety analysis revealed so much better results in the dual treatment group that the study was stopped. A total of 83 couples were assigned to the control group and 81 to the partner-treated group.
How impressive were the results? In the control group, 63% of women had a recurrence of BV within 12 weeks while it was 35% in the dual treatment group (I would be remiss not to point out that you never see these kinds of results for supplements or this caliber of study… ever… just sayin’). Pretty impressive.
There are some very important caveats:
80% of men were uncircumcised. Circumcision is associated with a lower risk of BV for the female partner, so the women in this study were at higher risk of recurrence. There is data to show there is more bacterial accumulation beneath the foreskin, so whether this antibiotic regimen will be as effective for circumcised men is simply unknown. This paper was underpowered to tell us if results differed by circumcision status.
The couples were in monogamous relationships for at least 8 weeks, so we can’t extrapolate these results to situations with more than one partner or short term partners.
A little over 25% of the women in both groups had an IUD. The copper IUD is a risk factor for recurrent bacterial vaginosis. The paper doesn’t break down how many had a copper IUD vs. a hormone IUD.
We don’t know the long term follow up. Meaning, will these results hold up at six months or a year? Getting BV to go away for 12 weeks is one thing (and an important thing), but keeping it away for six months or longer would be even better!
We don’t know how this routine might perform for reducing the risk of recurrent BV versus condom use.
We don’t know if repeated doses, such as male treatment once a week per month might help further reduce recurrences.
We don’t know if the results will be the same for women in racial or ethnic groups that were not represented in the study. This matters as the risk of BV and recurrence can vary. For example, in North America, African American and Hispanic women have the highest rates of bacterial vaginosis.
Compliance of the male partners affected the results; the partners of the men who were 100% adherent to the therapy had the lowest rate of recurrence. From an overall compliance standpoint, 14% of the men reported using less than 70% of the prescribed doses.
From a research and a clinical perspective, this is very exciting. Proving that treating the male partner supports the hypothesis that bacteria on the penis play a role in bacterial vaginosis. Hopefully, this study will lead to more studies that can answer some of the questions and caveats raised above. Also, we don’t know if the oral antibiotic plus topical antibiotic are both needed or if perhaps penile application of topical clindamycin might be sufficient.
Until we have more information, based on the strength of the study, I think people with recurrent BV who are in a monogamous relationship should have their partners treated with this double antibiotic combination, whether their partners are circumcised or not, as the evidence is compelling.
You might wonder about choosing a new therapy based on a single study, and that’s valid, but if we step back, this isn’t just a single study, there is a process here. Some men are known to be colonized with bacterial vaginosis associated bacteria (BVAB), so the hypothesis about treating this bacteria to improve outcomes regarding bacterial vaginosis was valid. As oral antibiotics have failed in three studies, the researchers did a pilot study where men were given oral antibiotics as well as the clindamycin antibiotic cream, and this combination reduced the BVAB bacteria on the penis. Now they had a proof of concept. The next step was the clinical trial we just discussed, which showed that the treatment had the intended effect or reducing bacterial vaginosis recurrence. And while we want to see this trial replicated in other populations as well as other studies to answer some of the questions (for example, does this work for men who are circumcised?), given the strength of the study, how it fits into the scientific literature, and the low risk of the therapy, adding treatment of male partners makes sense. All the while remaining open to what other studies might reveal.
As an aside, I have often grumbled from time to time about menopause influencers making big deals about pilot studies, and so it’s great to have an example here showing what should happen. When the pilot study had promising results, the researchers didn’t turn to Instagram to flog the therapy, no, they produced a quality clinic trial, which will hopefully spark a new line of research into treating bacterial vaginosis and preventing recurrence.
References
.
Muzny CA, Balkus J, Mitchell C, et al. Diagnosis and management of bacterial vaginosis: summary of evidence reviewed for the 2021 Centers for Disease Control and Prevention sexually transmitted infections treatment guidelines. Clin Infect Dis 2022; 74: Suppl_2: S144-S151.
Muzny CA, Taylor CM, Swords WE, Tamhane A, Chattopadhyay D, Cerca N, Schwebke JR. An Updated Conceptual Model on the Pathogenesis of Bacterial Vaginosis. J Infect Dis. 2019 Sep 26;220(9):1399-1405. doi: 10.1093/infdis/jiz342. PMID: 31369673; PMCID: PMC6761952
Muzny CA, Sobel JD. Bacterial Vaginosis — Time to Treat Male Partners. N Engl J Med 2025;392:1026-1027
Mehta SD. Systematic review of randomized trials of treatment of male sexual partners for improved bacteria vaginosis outcomes in women. Sex Transm Dis 2012; 39: 822-30.
Schwebke JR, Lensing SY, Lee J, et al. Treatment of male sexual partners of women with bacterial vaginosis: a randomized, double-blind, placebo-controlled trial. Clin Infect Dis 2021; 73(3): e672-e679.
Vodstrcil LA, Plummer EL, Fairley CK, et al. Male-partner treatment to prevent recurrence of bacterial vaginosis. N Engl J Med 2025; 392: 947-57.



Great analysis. As soon as I saw the NYTimes piece, I hoped you would write about the new study.
Thank you for this analysis, and I am so glad BV is finally being taken more seriously. Since the second Obama Administration, I have been in an on-and-off letter-writing battle with the CDC over their BV web page, which advises that women can reduce their risk of BV by "not having sex." While this advice may be factually accurate, I noted that their web page on malaria did not advise people to avoid going to malaria-infested areas in order to avoid contracting malaria, but instead provided actually useful advice on how to visit such places more safely. I used to believe that, with persistence, I would eventually be able to get them to change this ridiculous advice, but I fear the situation is hopeless how.