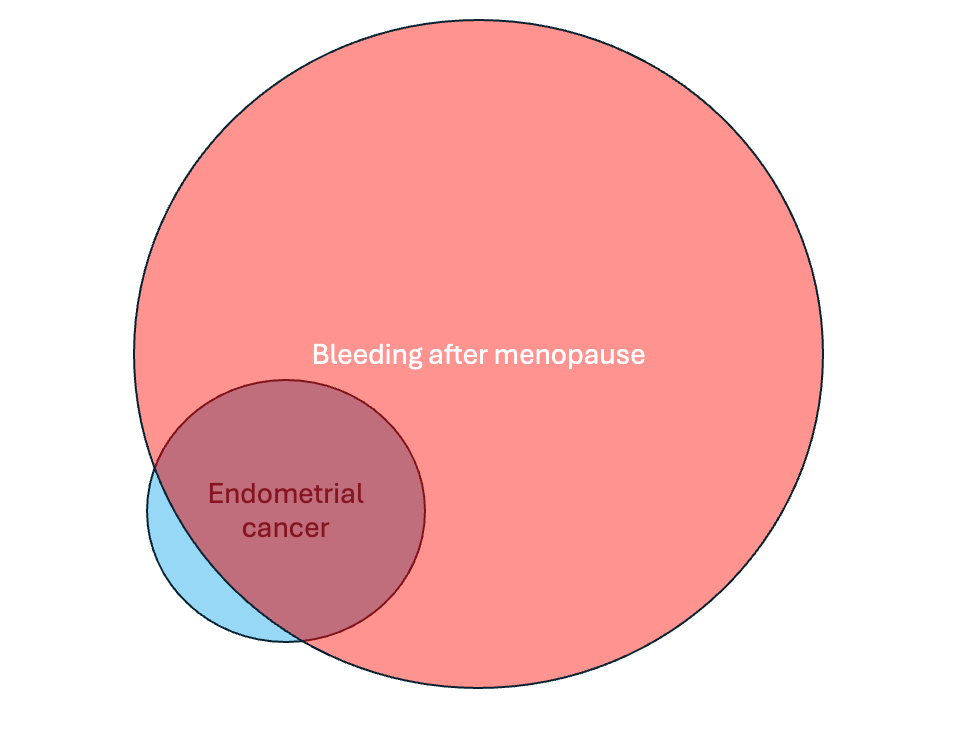
Bleeding after menopause should always be taken seriously, whether someone is on menopause hormone therapy (MHT) or not. There are many causes, and while most are benign, the risk of endometrial cancer for women with bleeding ranges from 1-14%, depending on the study. If you approach the statistics another way and look at women with endometrial cancer, about 90% of them had at least one episode of bleeding after menopause before they were diagnosed. This means it is important to rule out endometrial cancer when this kind of bleeding occurs.
One way to help determine if bleeding after menopause is concerning is by measuring the thickness of the uterine lining (endometrium) with a transvaginal ultrasound (an ultrasound with the probe in the vagina). If the thickness of the lining is ≤ 4 mm, the risk of endometrial cancer is believed to be < 1%. One study estimated that if 339 women with bleeding after menopause have an ultrasound and their uterine lining is ≤ 4 mm, only one of them will have cancer.
For most people, a physical exam and an endometrial thickness on ultrasound of ≤ 4 mm is enough of an initial investigation, although there are important exceptions, and so there are times when a tissue sample is needed so a pathologist can evaluate the tissue under a microscope to look for precancerous or cancerous cells. For example, recurrent bleeding (basically, you get a one-time evaluation of bleeding with the ultrasound, and if the bleeding persists, then more testing is needed); fibroids, which are benign tumors in the uterus that can distort the lining, making the measurement unreliable; or significant risk factors for endometrial cancer, such as taking estrogen without a progestogen.
People need to know that this ≤ 4 mm measurement applies only when there is bleeding after menopause; the implications of a thicker uterine lining are different when there is no bleeding. If an ultrasound is done for a reason other than bleeding and the uterine lining is > 4 mm, the cancer risk isn't the same. The American College of Obstetrics and Gynecology (ACOG) guidelines quote a study where 1,750 women without symptoms had an ultrasound, and when the thickness of the endometrium was ≤ 6 mm, only one cancer and four precancers were identified. Some studies suggest that 10 mm is an acceptable cut-off when there isn't any bleeding or other symptoms. As with most things, ultrasound findings must be put in context for the individual patient. The methods often vary from study to study, making a direct comparison hard. Still, the takeaway here for our purposes is that the thickness of the lining means more when there is bleeding and that a cut off ≤ 6 mm for women with no bleeding should miss very few cancers.
Concerns have been raised that ultrasound evaluation of the uterine lining may not be as effective a screening tool for Black women, and a recent modeling study suggested transvaginal ultrasound may miss more than four times more cases of endometrial cancer for Black women as compared with White women. This is an important and concerning finding, as Black women are almost twice as likely to die from endometrial cancer compared with White women. An ineffective screening tool would contribute to delays in diagnosis.
A new study provides even more information about ultrasound as a screening tool for endometrial cancer for Black individuals, and it’s important to get this information out. Investigators looked at the medical records of 1494 Black patients who had a hysterectomy from 10 medical centers and who had previously had a transvaginal ultrasound within the past 24 months. Of this group, 210 were ultimately diagnosed with endometrial cancer. The investigators looked at risk factors, such as age and body mass index, and the symptoms that prompted the original investigation, and more cancers than expected were identified among patients who would have otherwise been considered low risk based on ultrasound.
It’s possible that for some of the people in the study, there were changes over time that led to endometrial cancer, meaning, for example, an ultrasound performed 20 months before a hysterectomy might have shown a thickness of ≤ 4 mm, but over the following months, cancer developed and if an ultrasound had been done closer to the surgery the results would now be concerning. To help account for this, the researchers also looked at the smaller subset of 612 people who had their ultrasound within 90 days of their hysterectomy. I think this is a better real-world reflection from a cancer screening perspective. For an ultrasound done within 90 days of hysterectomy, the findings were a little better, but not much:
2.8% of cancers had an endometrial stripe of < 3 mm
7.7% of cancers had an endometrial stripe of < 4 mm
8.4% of cancers had an endometrial stripe of < 5 mm
Now, this data looks at everyone, including people who were not bleeding. What about when there was bleeding?
There were 161 cases of endometrial cancer among the 275 people with bleeding after menopause. A concerning number had a thin endometrium that wouldn’t otherwise be considered suspicious:
4.3% of endometrial cancers occurred with an endometrial thickness < 3 mm
10.6% with a thickness of < 4 mm
12.4% with a thickness < 5 mm
If someone had bleeding and an ultrasound showed an endometrial thickness of < 5 mm, there was only a 56% chance that the negative test result would be accurate. Which is about as good as flipping a coin. While the number of patients was small, ultrasound was not a good predictive tool for ruling out cancer when there was bleeding, whether the endometrial thickness was < 5 mm, < 4 mm, or even < 3 mm.
The researchers tried to find factors that made the ultrasound more or less reliable. Body mass index didn’t have a big impact. As expected, fibroids that obscured the ability of the ultrasound to evaluate the lining resulted in more missed cancers. Interestingly, a diagnosis of pelvic pain also meant that the ultrasound was likely to be less reliable. One hypothesis raised in the paper is that when women have pelvic pain, it may be more difficult for them to tolerate the ultrasound, so the scan wasn’t technically as good.
This study is retrospective, so it can’t answer all of our questions. The researchers had to review the charts for the ultrasound results, which were not recorded uniformly. Sometimes, it was a full radiology report, but other times, a doctor summarized the findings in a note, so there may be errors in how the ultrasound results were recorded. Because the ultrasounds were not done as part of a study, it’s also possible the techniques varied, and some of the ultrasounds missed cancers they should have picked up.
Despite these limitations, which are inherent in retrospective studies, this work is very important and suggests that endometrial thickness performs poorly in investigating bleeding after menopause for Black individuals. Until we have a prospective study that informs us otherwise, I agree with the authors that Black individuals should not rely on an ultrasound to evaluate bleeding after menopause and should also have tissue sampling.
References
The role of transvaginal ultrasonography in evaluating the endometrium of women with postmenopausal bleeding. ACOG Committee Opinion No. 734. American College of Obstetricians and Gynecologists. Obstet Gynecol 2018;131:e124–9.
Clarke MA, Devesa SS, Hammer A, Wentzensen N. Racial and Ethnic Differences in Hysterectomy-Corrected Uterine Corpus Cancer Mortality by Stage and Histologic Subtype. JAMA Oncol. 2022 Jun 1;8(6):895-903. doi: 10.1001/jamaoncol.2022.0009. PMID: 35511145; PMCID: PMC9073658.
Whetstone S, Burke W, Sheth SS, Brooks R, Cavens A, Huber-Keener K, Scott DM, Worly B, Chelmow D. Health Disparities in Uterine Cancer: Report From the Uterine Cancer Evidence Review Conference. Obstet Gynecol. 2022 Apr 1;139(4):645-659. doi: 10.1097/AOG.0000000000004710. Epub 2022 Mar 10. PMID: 35272301; PMCID: PMC8936152.
Doll KM, Khor S, Odem-Davis K, He H, Wolff EM, Flum DR, Ramsey SD, Goff BA. Role of bleeding recognition and evaluation in Black-White disparities in endometrial cancer. Am J Obstet Gynecol. 2018 Dec;219(6):593.e1-593.e14. doi: 10.1016/j.ajog.2018.09.040. Epub 2018 Oct 3. PMID: 30291839.
KM Doll, SS Romano, EE Marsh, et al. Estimated Performance of Transvaginal Ultrasonography for Evaluation of Postmenopausal Bleeding in a Simulated Cohort of Black and White Women in the US. JAMA Oncol. 2021;7(8):1158-1165.
KM Doll KM, Pike M, Alson J, et al. Endometrial Thickness as Diagnostic Triage for Endometrial Cancer Among Black Individuals. JAMA Oncol. Published online June 27, 2024. doi:10.1001/jamaoncol.2024.1891





So for this particular article women are adult human females? How refreshing not to have to read about "bleeders"! I hope this means that you have reconsidered your opinion, Dr. Gunter, that an individual can simply declare their biological sex and that the rest of the world must uncritically accept that as fact .
Would being on progesterone mask cancer as it prevents bleeding if on a daily dose? And what if your lining is thicker, say in the 6mm-9 mm range? How often and what kind testing is indicated in that circumstance? Would it be safer to just have a hysterectomy vs risking a missed cancer?