Mapping Testosterone Levels Through Midlife and Menopause
A new study offer more clarity
There is a new study that is hot off the press about testosterone levels and menopause. It’s well done and from a group that regularly produces good data, so I am eager to share it.
This is an important study because there is a lot of misinformation about testosterone and menopause, and social media plays an oversized role. There are menoinfluencers who, unfortunately, spread the message that testosterone levels drop in the menopause transition, and hence it should be replaced. “After all,” they say, “We’re just giving women what they’ve lost” and women “shouldn’t be afraid of their natural hormones.”
The data that we have had until now has not supported the idea that testosterone levels change in any relation to the menopause transition; instead, they follow an age-related decline, with an increase again around age 70. I’ve written about that previously here. The primary limitation of these studies is that most have employed immunoassays, which lack precision at the lower levels typically found in women. There is a study using liquid chromatography tandem mass spectrometry (LC-MS/MS), the gold standard for measuring testosterone in women, which found that from ages 18 to 39, levels dropped by 25% in an age-related decline, but that doesn’t help us understand the menopause transition.
Enter the new study, which uses LC-MS/MS to measure testosterone levels in a large cohort of women aged 40-69 from The Australian Women’s Midlife Years (AMY) Study. Some aspects of the study that make it strong include:
The investigators measured testosterone along with androstenedione and DHEA, which are hormones that the body converts into testosterone. They also measured sex hormone binding globulin (SHBG).
They excluded women taking hormones and those with medical conditions that might affect hormone levels.
They had data from 1,104 women.
Menopausal stage was determined using specific criteria. They classified women as:
Premenopausal
Perimenopausal
Menopausal and < 55 years
Menopausal and ≥ 55 years.
What Did the Researchers Find?
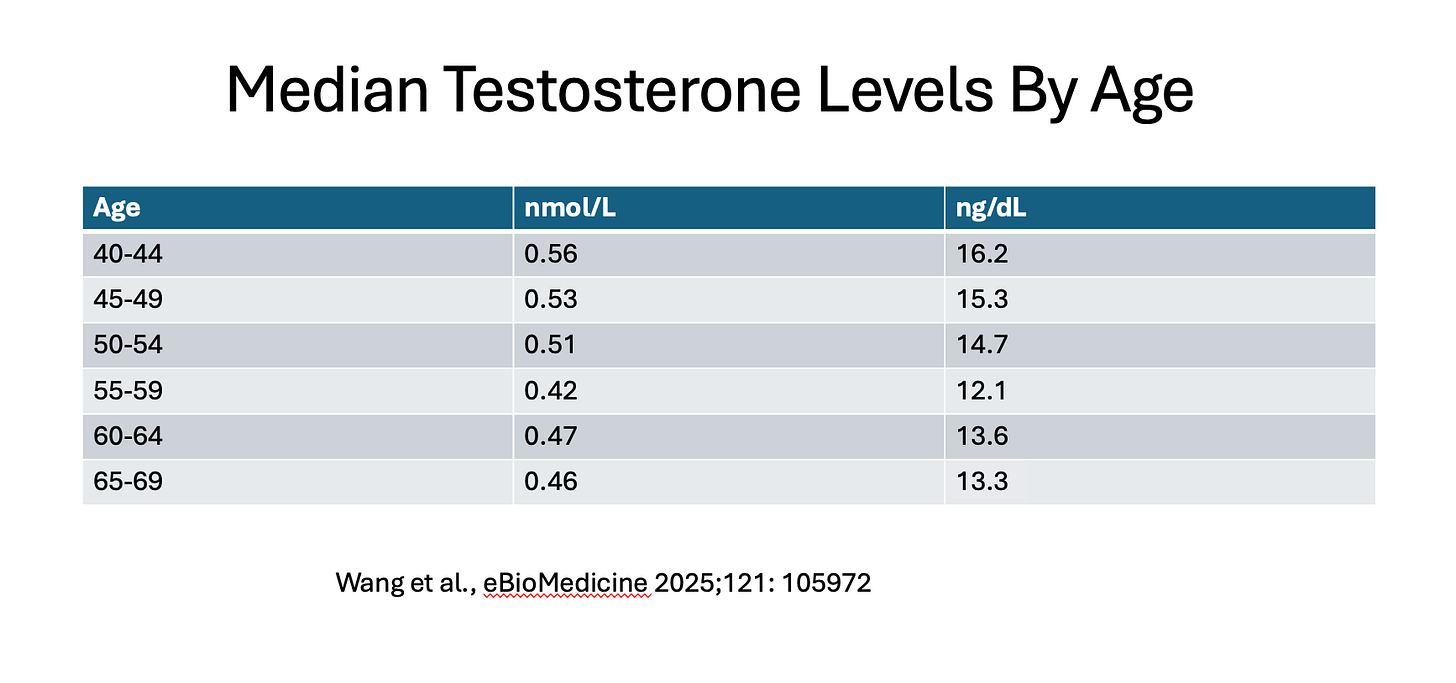
Testosterone levels declined from age 40 until age 58-59, when they hit their lowest. Over this time frame, testosterone levels dropped by about 25%. There was no relation between menopause status and testosterone, and the researchers were able to conclude this because they controlled for reproductive aging. After age 58-59, there was a gradual increase in testosterone, but not back to the levels at age 40.
Here are the median values by age group in both nmol/L and ng/dL from the study:
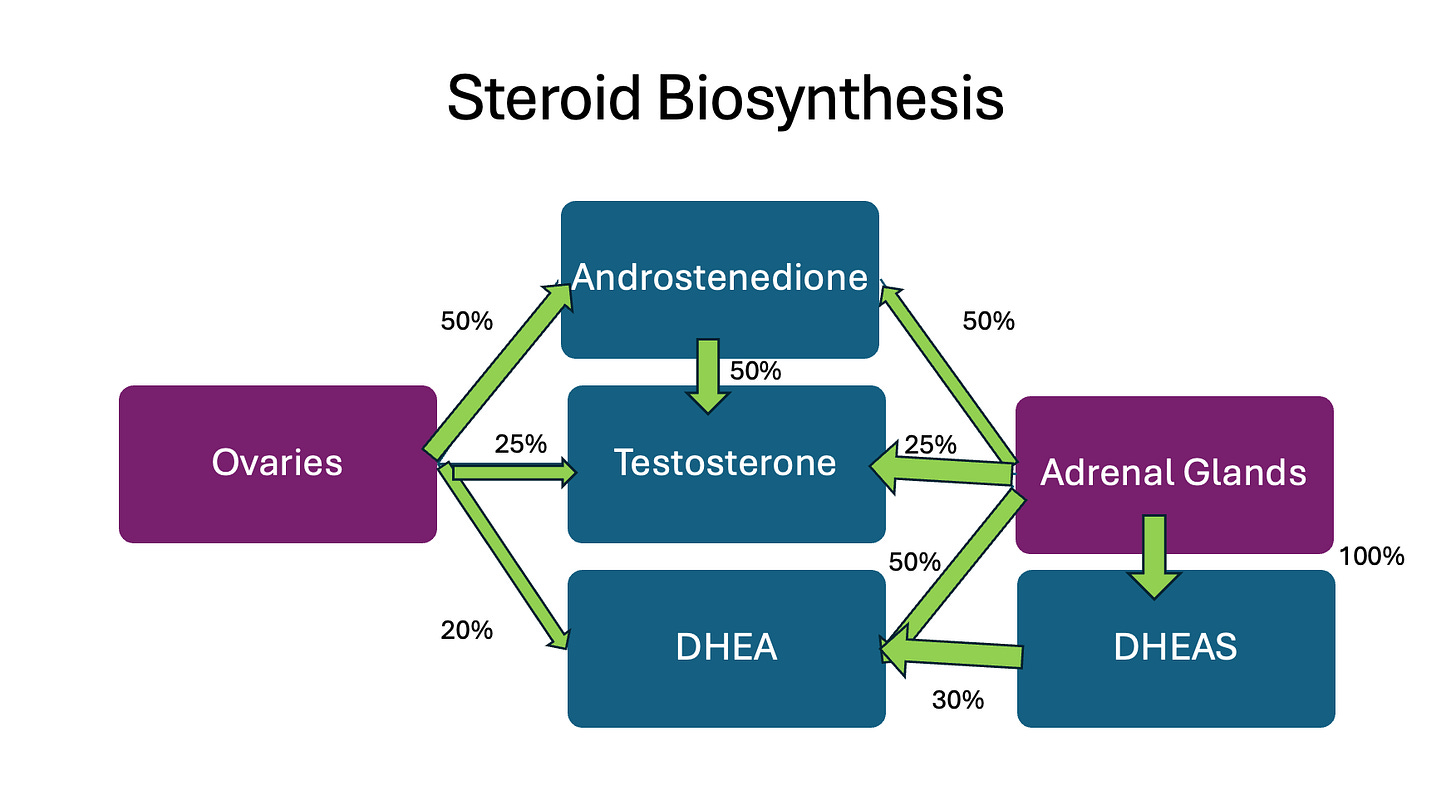
There was also an age-related decline in DHEA. In contrast, androstenedione levels decreased in relation to menopause. The authors felt this fit with what we know about steroid production (see chart below).
It makes sense that androstenedione levels drop in relation to menopause, as 50% is produced by the ovaries. On the other hand, no decrease in DHEA related to menopause was observed, which fits with what we know about steroid hormones, as the ovaries only produce about 20% of DHEA.
Why don’t testosterone levels drop in menopause if 25% of it comes from the ovary and the other 25% from androstenedione made by the ovary? The ovaries continue to produce some testosterone after menopause. In one study, the amount of testosterone coming from the ovaries after menopause was 24-fold higher than the testosterone in the general circulation (the researchers took blood from the ovarian veins during surgery, right before hysterectomy, and compared that with the testosterone in the general circulation). Granted, it’s a small study, and they used radioimmunoassays, so it needs to be replicated with more accurate tests. But we also know that women who have their ovaries removed typically have lower levels of testosterone. In addition to testosterone from ovaries after menopause, DHEA is still being produced and is converted into testosterone.
Some Interesting Thoughts from the Authors
They note that in early perimenopause, there is a higher incidence of disorders of desire and arousal than in premenopause. Yet, there is no meaningful change in testosterone levels between these two groups. As a result, these findings do not support the use of testosterone for libido or arousal-related concerns in the menopause transition.
They note that the lowest levels of testosterone are seen at ages 58-59, which corresponds with “the peak prevalence of low sexual desire, arousal, and sexual self-image.” This does support the use of testosterone to treat disorders of sexual desire and arousal for women who are postmenopausal and who are distressed by these changes and desire treatment.
They offer caution that the lowest levels of testosterone at ages 59-59, “should not be interpreted as justification for testosterone treatment of females of this age” for other reasons outside of libido/desire, as “randomised placebo-controlled trials have not shown testosterone supplementation confers other health benefits, such as prevention of muscle loss, cognitive benefits or improved mood, or increased bone density, with the caveat that many studies reporting these outcomes had major design limitations.” It is important to emphasize that there is no level where testosterone for women is considered too low. This is not like thyroid hormone or iron, where we know the body needs a specific level.
There is a lot of interest in understanding why testosterone levels naturally rise around age 60. Some data show that the women who don’t get that rise are more likely to have reduced grip strength, have more depressive symptoms, and are more likely to have cardiovascular disease. However, correlation does not necessarily mean causation, and we don’t know if this is cause and effect, so people should not jump to conclusions. It’s just as possible that depression or cardiovascular disease result in lower testosterone levels or that physical activity, which reduces cardiovascular disease risk and can treat depression, raises testosterone. Further research is required to elucidate the physiology underlying the later-in-life increase in testosterone.
The Caveat
This is a cross-sectional study, meaning women were not followed over time. We assume that the groups of women are pretty similar based on all of the screening and being matched for the stage of menopause. Still, it’s always possible that in a longitudinal study, there may be different results.
While longitudinal studies are ideal, following a large group of women over approximately thirty years and retaining enough participants to have sufficient data would be a significant undertaking and almost impossible.
Summing It All Up
Understanding what actually happens to testosterone across the menopause transition helps us separate evidence from influencer fantasy and sales pitches. The takeaway? For women, testosterone levels decline gradually with age, not because of menopause, and we should use the data we have to guide testosterone therapy based on science, not social media marketing.
World Menopause Day
Tomorrow, October 18, is World Menopause Day. In recognition, I will be doing a Substack Live at 9 am Pacific Time/Noon Eastern. I’ll be discussing the International Menopause Society White Paper on Lifestyle Medicine and Menopause, the Consumer Reports story on lead in protein powders, answering some questions from the community, and taking live questions. Hope to see you then!
References
Yuanyuan Wang, Rakibul M. Islam, Molly Bond, Susan R. Davis. Testosterone and pre-androgens by age and menopausal stage at midlife: findings from a cross-sectional study, eBioMedicine, Volume 121, 2025, 105972, ISSN 2352-3964.
Fogle RH, Stanczyk FZ, Zhang X, Paulson RJ. Ovarian androgen production in postmenopausal women. J Clin Endocrinol Metab. 2007 Aug;92(8):3040-3. doi: 10.1210/jc.2007-0581. Epub 2007 May 22. PMID: 17519304.



Thank you again for summarizing this. much appreciated.
Thank you for this. This is so important. I have seen an uptick of women taking testosterone and this helps to understand when it is indicated and when it is not. Thank you for providing accurate information, evidence and dispelling myths.