I’ve been waiting for this one for a while. I had heard through the medical grapevine that the studies looked good and was hoping it was just a matter of time. And it was!
This week a brand new drug was approved for vaginal yeast infections called ibrexafungerp (no idea how to pronounce it), which will be marketed under the name Brexafemme. What is exciting about this drug is that it works in a completely different way than the antifungals (yeast medications) that are currently available. This means it will be an option for women who have yeast that is resistant to the currently available medications, known as azoles, or for women who are allergic to azoles.
Some Background on Azoles
You may know these drugs by the following names: miconazole (Monistat), clotrimazole (Lotromin), and terconazole (Terazol), all of which are topical; and the oral fluconazole (also known as Diflucan). The azoles inhibit an enzyme called lanosterol 14-alpha-demethylase, which is essential for making ergosterol, a lipid that is an essential component of fungal cell membranes. Azoles are fungistatic, meaning they inhibit the growth of yeast, they don’t directly kill it. Basically, the yeast is sufficiently stunned and the immune system takes it from there.
Being fungistatic may be one reason why yeast may recur after treatment with azole medications. This is because a local disturbance in the vaginal immune system (which includes the microbiome) may be part of the reason the yeast has overgrown and caused symptoms in the first place. So when the yeast is stunned by the fluconazole the body may not be able to take it from there, as it were, and so the yeast comes back. The other reason why azole medications fail is resistance, meaning the yeast has developed ways to defend against these medications or the yeast is naturally resistant to the azoles. Azole resistance is a growing concern in vaginal yeast infections and failure of the azole medications is one reason many women turn to vaginal boric acid. Another reason people turn to boric acid is misinformation online. If you want to read more about boric acid, please check out this article of mine from a few weeks ago
Ibrexafungerp
I admit it’s a mouthful, so we’ll use it’s trade name Brexafemme. This is a glucan synthase inhibitor, so it works in an entirely different way than the azole drugs. It is also fungicidal, meaning it kills the yeast, which is very exciting. It has been shown in studies to not only kill Candida albicans, the most common yeast that causes vaginal infections, but to also work against some of the other yeast types that aren’t as well treated or are naturally resistant to the azoles, such as Candida glabrata. As there are no commercially available products for vaginal infections due to yeast that has acquired resistance to azoles or is naturally resistant to azoles, Brexafemme could be a real game changer. Right now in some clinics like mine that specialize in hard to treat yeast about 10% of the yeast can’t be treated with azole medications.
The dose of Brexafemme is 300 mg twice a day taken on one day. It should not be used during pregnancy as during animal studies it caused malformations in fetal rabbits. It is important to note that a significant percentage of people had side effects with Bexafemme, the most common were diarrhea (16.7%), nausea (11.9%), and abdominal pain (11.4%). For comparison, among people who took a placebo, those numbers were 3.3%, 4.0% and 5.1% respectively. The product monograph is here for those who want to read more.
So how well does Bexafemme work? There were two phase 3 studies that led to approval. In one study, 63.3% of women had resolution of their symptoms at 10 days (short term success) and 73.9% at day 25. In this study 58.5% of women had a negative culture at their short term follow up visit, meaning lab tests showed they had cleared the yeast. The other trial showed 50.5% of women had resolution of symptoms at 10 days and the yeast cleared on culture (lab testing) for 49.5%
This is a lower success rate than with the drugs currently available. For example, in one study with fluconazole the short term success for clearing yeast (negative culture at 5-16 days) was 85% and with clotrimazole (a topical) it was 81%. The number of women who responded with clinical improvement (meaning they feel better) to Bexafemme is also lower than the data we have with both fluconazole and the topical azoles—both of which typically have short term success rates in the 90% or higher range. However, comparing results from drugs between studies isn’t necessarily accurate and much of the data we have on azoles is older when resistance was less of an issue. To really compare Brexafemme with fluconazole and the over-the-counter azoles we need head-to-head (vagina-to-vagina?) studies, and we don’t have those yet.
Bottom Line
Brexafemme looks like a welcome addition for women with azole-resistant yeast, rapidly recurring yeast (within 1-2 months of therapy), or who are allergic to the azoles. Having an option other than boric acid will be fantastic. It will be important to keep an eye out for side-effects and of course to make sure performance in the real world matches what we see in the studies. For every day run of the mill vaginal yeast Brexafemme doesn’t currently look like a replacement for fluconazole (Diflucan) or the over-the-counter medications as the actual cure rates by culture are lower than what we have seen historically with the azoles, but as more data emergences that may well change.
Brexafemme looks like it’s going to help fill an important gap in management of yeast infections, and over time we will know more about how it stacks up vagina-to-vagina against what we already have available. But honestly, having a new antifungal that is fungicidal is great…actually, it’s really exciting! I’ve heard there is another possibly even better antifungal finishing up phase 3 trials now, so hopefully there will be more exciting things to report. But it’s early days, and until you see the data you don’t really know.
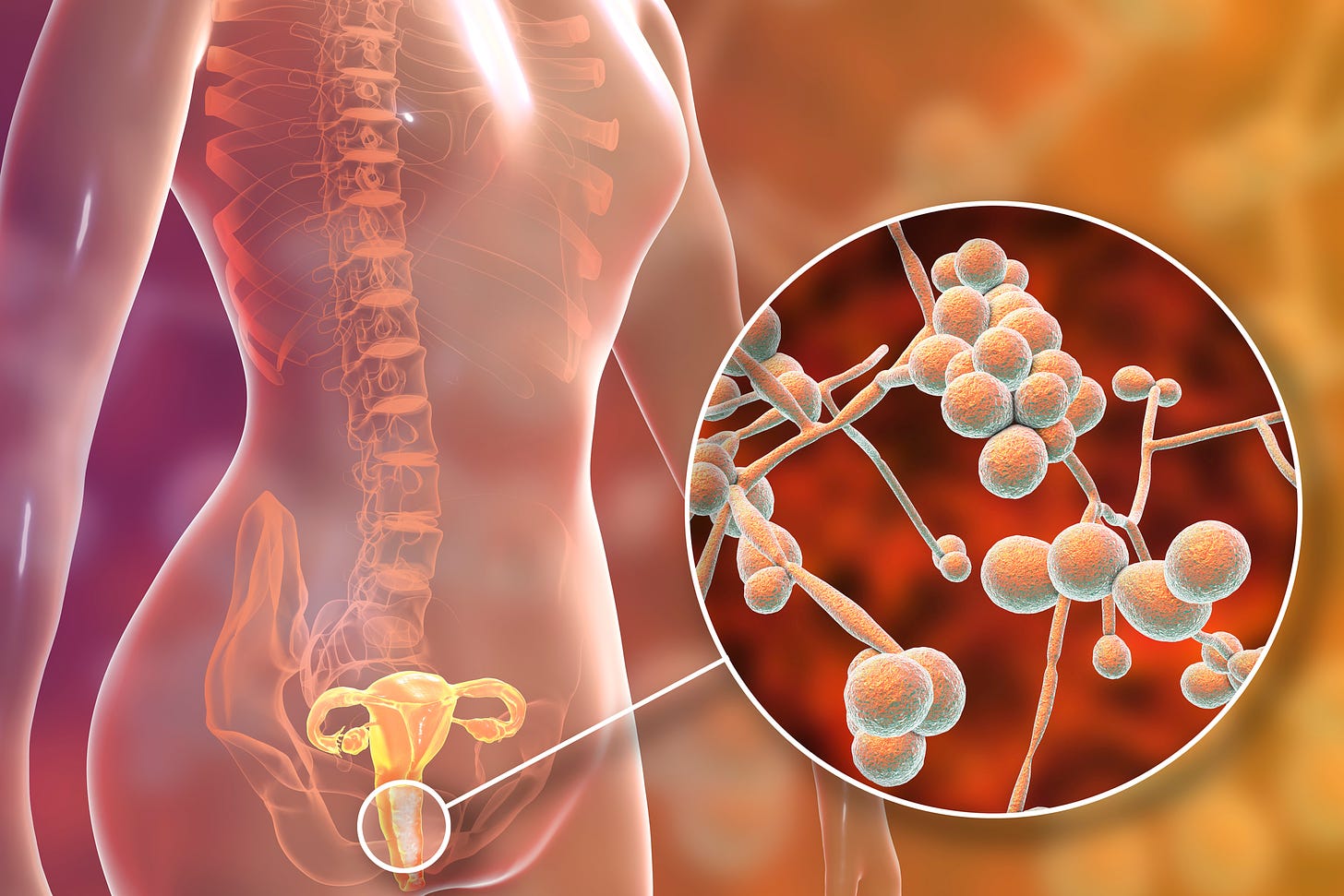
And for those who are interested, this is what yeast looks like under the microscope.





Hi Dr. Jen. I subscribed to you because you’ve helped me understand vaginal health well. I suffer from recurrent vulvovaginal candida as a 21 year old woman with no other health conditions. It started a year ago after an episode of BV and getting a copper IUD (that I got removed immediately after). I do all the right things: cotton underwear, avoid douching/fragrance, only wash with water, etc… I’ve already undergone long-term therapy this year, and I am about to again because the infection returned. Is there any advice you can offer me, please? The gynecologists in my area are not super helpful. Please and thank you.