It’s been an interesting week at the annual meeting of the Menopause Society. There were great reviews, complex deep dives, exciting new research, and a few points of aggravation—basically, your average medical meeting.
I need time to mull over some of the lectures and do some more reading before I can do them justice (sometimes talks lead to more questions than answers). However, one talk stood out as having some practical content I could get out to you quickly: colon cancer screening, given by Dr. Cindy Yoshida, MD.
Special thanks to my gastroenterologist buddy, Dr. Kaveh Hoda, who helped me fact-check. Unlike journal articles, talks at meetings aren’t peer-reviewed, so I always double-check key facts or anything controversial before bringing that information to you. This felt straightforward, a testimony to Dr. Yoshida’s great talk and clear communication, but since this isn’t my area of expertise, it’s always nice to be able to phone a friend!
Colon Cancer Screening, the State of Affairs
The new U.S. guidelines are to start screening people at average risk for colon cancer at age 45. This doesn’t apply to people with a family history, those who have inflammatory bowel disease or other risk factors, or those with bowel symptoms. This means no symptoms; your age is the only reason to check.
In the United States, only one-third of people eligible for this screening get screened, which is pretty dismal. A study shared by Dr. Yoshida showed that when 83% of eligible individuals are screened, the number of cases of colon cancer decreases by 26%, and colon cancer deaths decrease by 52%. That’s a pretty impressive case for screening.
There are three main methods for colon cancer screening in the United States for people at average risk:
FIT (Fecal Immunochemical Test). This test is done once a year and involves sampling stool and can be done at home. You put special paper in the toilet, poop onto the paper, stick a small plastic wand into your poop, and then in a small bottle, and mail. The FIT test detects hemoglobin (the major oxygen-carrying protein in blood) in the stool. When positive, this suggests the presence of microscopic blood, which could be from a precancer or cancer. When a FIT test is positive, a colonoscopy is needed.
sDNA-FIT (Cologuard®). This test is done every 1-3 years and is also a stool-based test that can be done at home, but it’s a bit more involved than FIT. You are given a special bucket that attaches to the toilet seat. Once you set that up, you pass your entire bowel movement into the bucket, add the supplied preservative, and then mail it in. This test detects DNA biomarkers for hemoglobin as well as using an antibody test (meaning, like FIT, it’s also a test for blood in the stool). When the sDNA-FIT is positive, a colonoscopy is needed. Apparently, false positive tests are a little higher compared with FIT.
Colonoscopy. Taking medication to clean out the colon and having a provider use a special camera to look inside to identify adenomas, which are precancerous lesions.
The FIT and sDNA-FIT are home tests, less expensive, don’t require a prep to clean out the colon, there is no time off work or school, and no one has to take time off to drive you home from a procedure. The disadvantage is if the test is positive, you need a colonoscopy. Also, their effectiveness as a screening tool is only as good as the ability to get in for a colonoscopy for those who screen positive.
The hassle of a colonoscopy is, well, the hassle of a colonoscopy. The prep, the day off work/school/away from home, the anesthesia, and the need for someone to drive you home. There are also rare but serious complications, which occur about as often as they do with surgical abortions, meaning they are very rare (and yet not ONE politician is worried about regulating colonoscopy for safety…I wonder why, she writes in sarcasm font). The benefit of a colonoscopy is any pre-cancers can be removed at the time, so it’s one and done.
Which Screening is Best?
I admit, I went into the lecture thinking colonoscopy would have far fewer deaths from colon cancer. I wouldn’t be surprised if a study somewhere says surgeons are biased about thinking procedures are always better than lab-based testing (she opines with some self-reflection).
While a single FIT or sDNA-FIT test misses more adenomas than a colonoscopy, with each year, their performance improves because the test keeps getting repeated (assuming they happen as often as they are supposed to and positive screens get in for a colonoscopy). This chart shared by the speaker shows years of life gained per 1000 people screened, which is a way of comparing one method of screening with another. You can see that FIT or sDNA-FIT every year and colonoscopy every 10 years are pretty close.
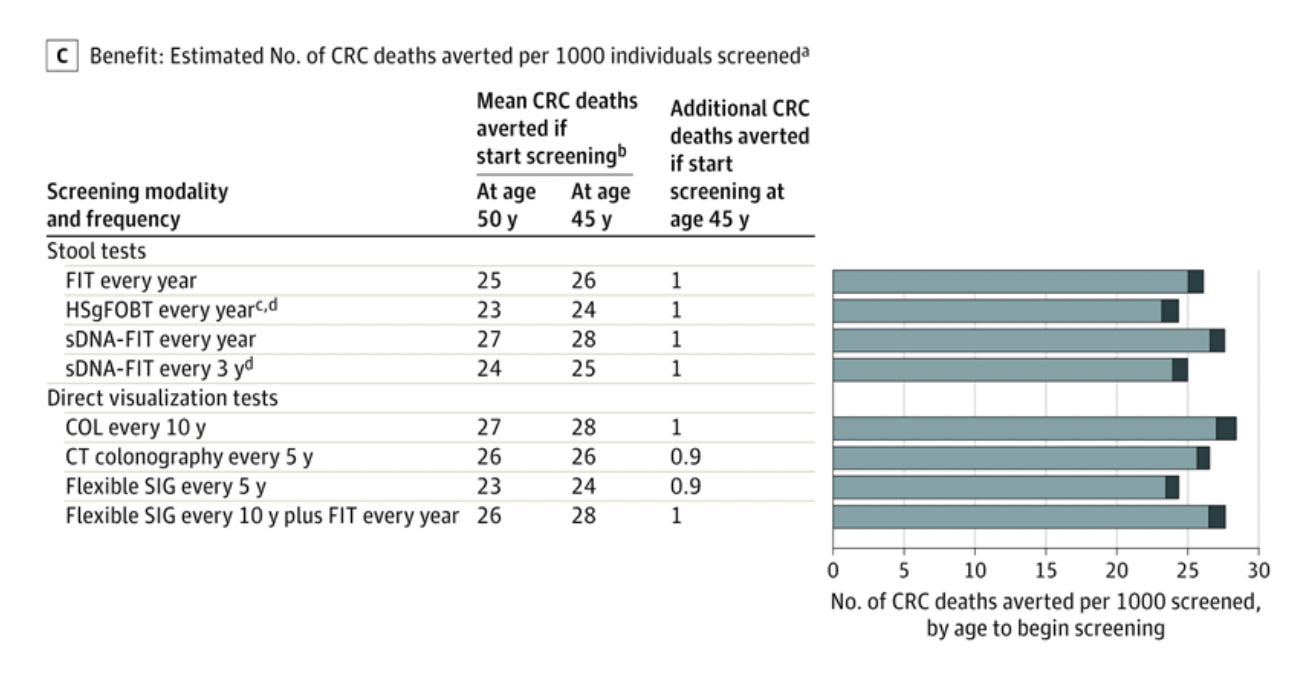
I found this other graph from the same source (USPSTF), and it explains the outcomes in a way that might be more relatable to non-gastroenterologists (like me!). For every 1,000 people screened, starting at age 45, 26 lives will be saved with yearly FIT tests, 28 with yearly sDNA-FIT, and 28 with a colonoscopy every 10 years.
When We Don’t Offer All Screening Methods, People Suffer
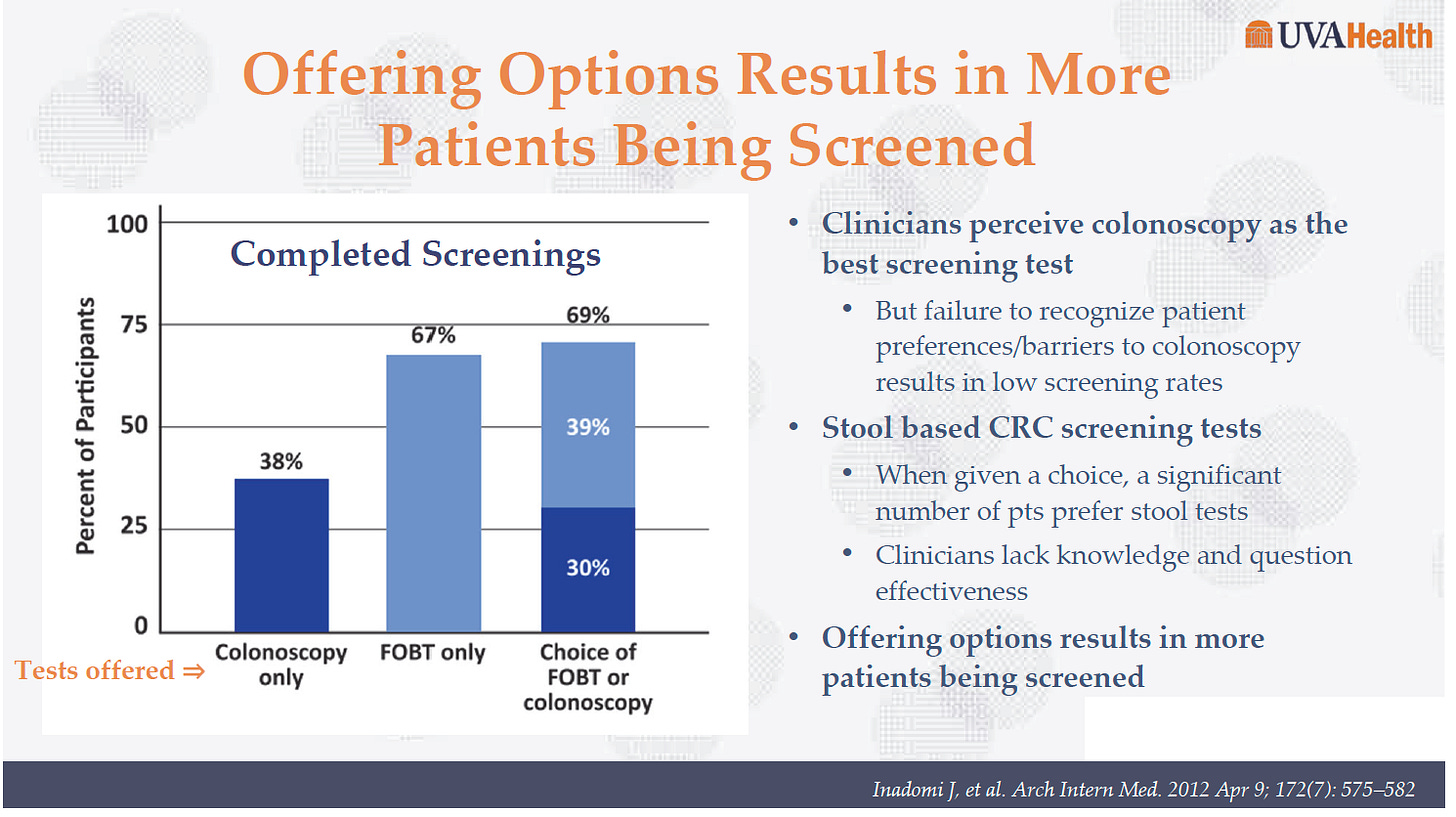
When providers only offer colonoscopy, 38% of people get screened for colon cancer. If we only offer stool-based testing, the screening rate jumps significantly. And if we offer the choice of home testing or colonoscopy, screening rates are the highest. It’s also clear lots of people prefer stool-based tests because when given a choice, that’s what many choose. The speaker suggested this might be due to people becoming very familiar with home testing, for example, via tests like 23andMe.
Something to Know About Colonoscopy
I did not know what I am about to tell you. Like it was totally new to me, and talking amongst other attendees, I was not the only one! Although, I’m sure it’s old news to gastroenterologists and colorectal surgeons.
FIT and sDNA-FIT are automated tests, so there is little opportunity for operator error (I knew this part). The error here is not getting people to test every year and not getting people in for their colonoscopy. And the quality of the follow-up colonoscopy if needed.
About the quality of the colonoscopy…detecting adenomas at colonoscopy depends on the prep quality and the operator's skill, so the rate varies. I suspected this part going into the lecture. Still, I did not know that the rate of detection of adenomas at screening colonoscopies is tracked in the United States as a quality measure. The denominator is colonoscopies for those age 50 and older that are done for routine screening as well as those done because of family history. Adenoma detection rates are important because they are predictive of developing colon cancer in the interval between screening. The higher the adenoma detection rate, the lower your chances of developing cancer over the next 10 years in the interval between screening colonoscopies. The speaker said the adenoma detection rate should be at least 30%. However, the current US guidelines recommend an adenoma detection rate of 30% for men and 20% for women. I’m not sure why women should accept a lower adenoma detection rate in the United States when the European guidelines are 25% for average-risk people age 50 and older, with no difference for men vs. women. I will try to find the answer, and if any GI docs follow me, please let me know. I hope it’s not *waves hands in the air out of frustration* inadequate studies involving women, which can be translated into the patriarchy.
One study suggests that gastroenterologists have the highest adenoma detection rate, followed closely by colorectal surgeons and then general surgeons, who had an adenoma detection rate of 18.4%. The adenoma detection rate should be the same for those 45 to < 50 years as it is for the 50 and up crowd. This means the new screening guidelines shouldn’t change the adenoma detection rate.
Summary
For people at average risk for colon cancer screening, ALL colon cancer screening is great colon cancer screening. The best test is the one that you can access and will do.
If you plan on going the colonoscopy route, ask for your colonoscopist’s adenoma detection rate. You have a right to know.
***
Stay tuned for more updates! I think I’ll post a list of “fast facts” that I picked up from various lectures at the meeting and then take a deeper dive into the lectures on breast density and on dementia. And coming up next in the hormone menoverse series is hormone types and doses. I know many of you have been waiting for this part of the series.
References
US Preventive Services Task Force. Screening for Colorectal Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2021;325(19):1965–1977. doi:10.1001/jama.2021.6238
Quality ID #343: Screening Colonoscopy Adenoma Detection Rate. https://qpp.cms.gov/docs/QPP_quality_measure_specifications/CQM-Measures/2019_Measure_343_MIPSCQM.pdf






another great informative post - thank you
Re: breast density- please! V. Interested in your learnings. I have dense breast but not sure what that means I should do for prevention tests. 🤷♀️ notified each year after my mammo about my dense breast but what next?